
RESPIRATORY ORGANS IN ANIMALS: Diverse Strategies for Gas Exchange
I. Overview of Respiratory Mechanisms:
- Adaptations Across Animal Groups:
- Varied Strategies:
- Different animal groups employ diverse mechanisms for gas exchange based on their habitats and organizational levels.
- Varied Strategies:
II. Lower Invertebrates:
- Diffusion-Based Respiration:
- Examples:
- Sponges, coelenterates, flatworms, etc.
- Mechanism:
- Exchange of O2 and CO2 occurs through simple diffusion over the entire body surface.
- Examples:
III. Earthworms and Insects:
- Moist Cuticle and Tracheal Tubes:
- Earthworms:
- Utilize their moist cuticle.
- Insects:
- Employ a network of tubes (tracheal tubes) to transport atmospheric air within the body.
- Earthworms:
IV. Aquatic Arthropods and Molluscs:
- Gill-Based Respiration:
- Mechanism:
- Utilization of vascularized structures called gills for gas exchange.
- Examples:
- Most aquatic arthropods and molluscs.
- Mechanism:
V. Terrestrial Forms:
- Lung-Based Respiration:
- Mechanism:
- Employ vascularized bags called lungs for the exchange of gases.
- Examples:
- Terrestrial vertebrates like amphibians, reptiles, birds, and mammals.
- Mechanism:
VI. Amphibians:
- Cutaneous Respiration:
- Additional Mechanism:
- Moist-skinned amphibians like frogs can respire through their skin (cutaneous respiration).
- Additional Mechanism:
VII. Vertebrates:
- Fish:
- Respiratory Organ:
- Gills.
- Respiratory Organ:
- Amphibians, Reptiles, Birds, Mammals:
- Respiratory Organ:
- Lungs.
- Respiratory Organ:
VIII. Adaptation to Environment:
- Tailored to Habitat:
- Animals exhibit respiratory adaptations in response to their specific environmental niches, ensuring efficient gas exchange.
HUMAN RESPIRATORY SYSTEM: An In-Depth Overview
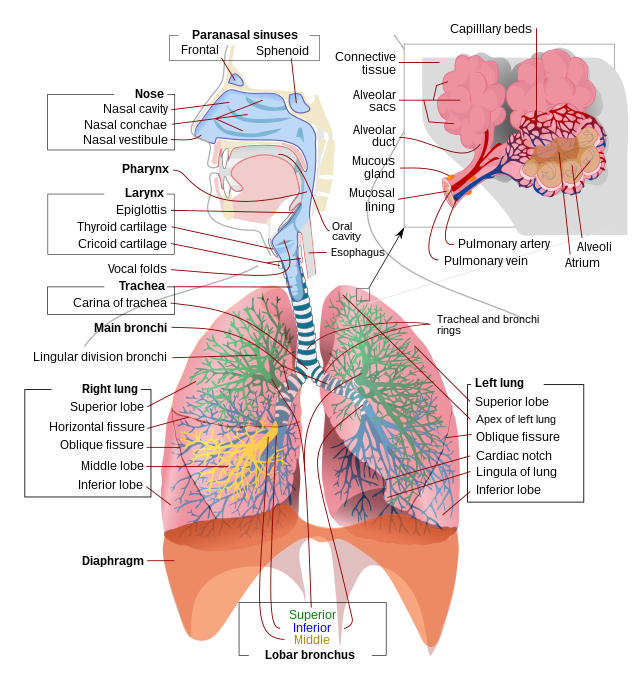
I. External Nostrils to Nasal Chamber:
- Nostrils:
- Pair of external nostrils above the upper lips.
- Nasal Passage and Chamber:
- Nostrils lead to the nasal passage, opening into the nasal chamber.
II. Nasal Chamber to Pharynx:
- Common Passage for Food and Air:
- Nasal chamber opens into the pharynx.
- Pharynx is a common passage for both food and air.
III. Pharynx to Larynx and Trachea:
- Larynx (Sound Box):
- Cartilaginous box aiding in sound production.
- Glottis can be covered by the epiglottis during swallowing to prevent food entry.
- Trachea:
- Straight tube extending to mid-thoracic cavity.
- Divides into right and left primary bronchi at the 5th thoracic vertebra.
IV. Bronchi and Bronchioles:
- Bronchi Division:
- Primary bronchi divide into secondary and tertiary bronchi.
- Further divisions lead to bronchioles, ending in terminal bronchioles.
- Cartilaginous Support:
- Incomplete cartilaginous rings support tracheae, primary, secondary, and tertiary bronchi.
V. Alveoli:
- Structure:
- Very thin, irregular-walled, vascularized bag-like structures.
- Location:
- Terminal bronchioles give rise to alveoli.
- Respiratory or Exchange Part:
- Site for diffusion of O2 and CO2 between blood and atmospheric air.
VI. Lungs and Pleura:
- Double-Layered Pleura:
- Covers two lungs.
- Pleural fluid reduces friction on lung surface.
- Thoracic Chamber:
- Formed dorsally by vertebral column, ventrally by sternum, laterally by ribs, and on the lower side by diaphragm.
- Thoracic chamber is anatomically air-tight.
VII. Respiratory Process:
- Breathing or Pulmonary Ventilation:
- Drawing in atmospheric air and releasing CO2-rich alveolar air.
- Diffusion of Gases:
- O2 and CO2 diffusion across the alveolar membrane.
- Transport of Gases:
- Gases transported by blood.
- Diffusion in Tissues:
- O2 and CO2 diffusion between blood and tissues.
- Utilization in Cells:
- Cells utilize O2 for catabolic reactions, releasing CO2.
VIII. Thoracic Cavity and Lung Volume:
- Anatomical Setup:
- Any change in thoracic cavity volume reflects in the pulmonary cavity.
- Essential for Breathing:
- Enables breathing as pulmonary volume cannot be directly altered.

IX. Key Respiratory Steps:
- Breathing
- Gas Diffusion
- Gas Transport
- Tissue Gas Diffusion
- Cellular Utilization
MECHANISM OF BREATHING: Understanding Inspiration and Expiration
I. Breathing Stages:
- Two Stages:
- Inspiration: Drawing in atmospheric air.
- Expiration: Releasing alveolar air.
II. Pressure Gradient:
- Pressure Difference:
- Movement of air results from a pressure gradient between lungs and atmosphere.
- Inspiration: Intra-pulmonary pressure < Atmospheric pressure.
- Expiration: Intra-pulmonary pressure > Atmospheric pressure.
III. Muscular Involvement:
- Muscles Involved:
- Diaphragm:
- Initiates inspiration by contracting.
- Increases thoracic chamber volume antero-posteriorly.
- External and Internal Intercostal Muscles:
- Contribute to volume increase dorso-ventrally.
- Diaphragm:
IV. Mechanism of Inspiration:
- Diaphragm Contraction:
- Increases thoracic chamber volume.
- External Intercostal Muscles:
- Lift up ribs and sternum.
- Increases thoracic volume dorso-ventrally.
- Volume Increase:
- Thoracic and pulmonary volume rise.
- Intra-pulmonary Pressure:
- Decreases below atmospheric pressure.
- Air Movement:
- Atmospheric air flows into lungs.
V. Mechanism of Expiration:
- Diaphragm and Muscles Relax:
- Return to normal positions.
- Volume Decrease:
- Thoracic and pulmonary volume decrease.
- Intra-pulmonary Pressure:
- Increases above atmospheric pressure.
- Air Expulsion:
- Air expelled from lungs.
VI. Additional Muscles:
- Abdominal Muscles:
- Assist in enhancing inspiration and expiration strength.
VII. Breathing Rate:
- Average Rate:
- A healthy human breathes 12-16 times/minute.
- Spirometer Usage:
- Estimates air volume involved in breathing movements.
- Assists in clinical pulmonary function assessment.

RESPIRATORY VOLUMES AND CAPACITIES: Understanding Lung Function
I. Respiratory Volumes:
- Tidal Volume (TV):
- The volume of air inhaled/exhaled during normal respiration.
- Approx. 500 mL.
- Inspiratory Reserve Volume (IRV):
- Additional air volume inspired by forceful inhalation.
- Averages 2500 mL to 3000 mL.
- Expiratory Reserve Volume (ERV):
- Additional air volume expired by forceful exhalation.
- Averages 1000 mL to 1100 mL.
- Residual Volume (RV):
- Air volume remaining in lungs after forceful exhalation.
- Averages 1100 mL to 1200 mL.
II. Respiratory Capacities:
- Inspiratory Capacity (IC):
- Total air volume a person can inhale after normal exhalation.
- Includes TV and IRV (TV + IRV).
- Expiratory Capacity (EC):
- Total air volume a person can exhale after normal inhalation.
- Includes TV and ERV (TV + ERV).
- Functional Residual Capacity (FRC):
- Air volume remaining in lungs after normal exhalation.
- Includes ERV and RV (ERV + RV).
- Vital Capacity (VC):
- Maximum air volume a person can inhale after forced exhalation.
- Includes ERV, TV, and IRV, or the maximum volume exhaled after forced inhalation.
- Total Lung Capacity (TLC):
- Total air volume in lungs after forced inhalation.
- Includes RV, ERV, TV, and IRV, or VC + RV.
EXCHANGE OF GASES IN THE RESPIRATORY SYSTEM: Alveolar Dynamics
I. Alveolar Exchange:
- Primary Sites for Gas Exchange:
- Alveoli: Main sites for gas exchange.
- The exchange also occurs between blood and tissues.
- Mechanism:
- Exchange is based on simple diffusion.
- Relies on pressure/concentration gradients.
- Solubility of gases and membrane thickness affect diffusion rates.
- Partial Pressure:
- The pressure of an individual gas in a gas mixture.
- Represented as pO2 (oxygen) and pCO2 (carbon dioxide).
II. Gas Exchange Data:
- Oxygen (O2):
- Concentration gradient from alveoli to blood and blood to tissues.
- Facilitates diffusion in both directions.
- Carbon Dioxide (CO2):
- Concentration gradient from tissues to blood and blood to alveoli.
- Higher solubility (20-25 times more than O2) enhances diffusion.
III. Diffusion Membrane:
- Components:
- Thin squamous epithelium of alveoli.
- Endothelium of alveolar capillaries.
- Basement substance (thin basement membrane) between them.
- Thickness:
- The total thickness is less than a millimeter.
- Favors efficient diffusion of O2 from alveoli to tissues and CO2 from tissues to alveoli.
TRANSPORT OF GASES IN THE BLOOD: Oxygen and Carbon Dioxide Dynamics
I. Oxygen Transport:
- Blood as the Medium:
- RBCs carry about 97% of O2.
- The remaining 3% is dissolved in plasma.
- Haemoglobin Interaction:
- Haemoglobin (iron-containing pigment in RBCs) reversibly binds with O2.
- Each hemoglobin molecule can carry up to four O2 molecules.
- Binding is influenced by pO2, pCO2, H+ concentration, and temperature.
- The oxygen Dissociation Curve (sigmoid) illustrates saturation with O2.
- Dissociation at Tissues:
- O2 binds in the lungs (high pO2, low pCO2, lower temperature).
- Dissociates at tissues (low pO2, high pCO2, higher temperature).
- Facilitates O2 delivery to tissues.
II. Carbon Dioxide Transport:
- Haemoglobin Interaction:
- About 20-25% of CO2 is carried by hemoglobin as carbamino-hemoglobin.
- Binding influenced by pCO2.
- Enzyme Facilitation:
- Carbonic anhydrase enzyme is present in high concentrations in RBCs.
- Catalyzes conversion of CO2 to bicarbonate (HCO3–) and H+.
- Reaction occurs at tissue and alveolar sites.
- Release at Alveoli:
- CO2 is trapped as bicarbonate in tissues.
- Released as CO2 at alveoli (low pCO2).
- Facilitates CO2 elimination.

REGULATION OF RESPIRATION: Neural and Chemical Control
I. Neural Regulation:
- Respiratory Rhythm Centre:
- Located in the medulla region of the brain.
- Primary regulator of respiratory rhythm.
- Pneumotaxic Centre:
- Located in the pons region of the brain.
- Modifies functions of the respiratory rhythm center.
- Regulates duration of inspiration, influencing respiratory rate.
- Chemosensitive Area:
- Adjacent to the rhythm center.
- Highly sensitive to CO2 and hydrogen ions.
- Activated by increased CO2 and H+, signaling adjustments in respiration.
II. Chemical Regulation:
- Chemosensitivity:
- The chemosensitive area responds to changes in CO2 and H+ concentration.
- Activation leads to adjustments in the respiratory process.
- Receptor Recognition:
- Receptors in the aortic arch and carotid artery.
- Recognize changes in CO2 and H+ concentration.
- Transmit signals to the rhythm center for corrective actions.
- Limited Role of Oxygen:
- Oxygen’s role in respiratory rhythm regulation is insignificant.
- Regulation primarily centered around CO2 and H+ levels.
DISORDERS OF THE RESPIRATORY SYSTEM
1. Asthma:
- Definition: Difficulty in breathing, accompanied by wheezing.
- Cause: Inflammation of bronchi and bronchioles.
- Symptoms:
- Wheezing sound during breathing.
- Constriction of airways.
- Management:
- Anti-inflammatory medications.
- Bronchodilators to relieve symptoms.
2. Emphysema:
- Definition: Chronic disorder with damage to alveolar walls.
- Cause: Mainly linked to cigarette smoking.
- Symptoms:
- Reduced respiratory surface area.
- Difficulty in exhaling.
- Management:
- Smoking cessation.
- Medications to ease symptoms.
3. Occupational Respiratory Disorders:
- Definition: Disorders resulting from occupational exposure.
- Cause: Prolonged exposure to dust in certain industries.
- Consequences:
- Dust exposure overwhelms the body’s defense mechanisms.
- Inflammation leads to fibrosis (fibrous tissue proliferation).
- Serious lung damage.
- Prevention:
- Workers should wear protective masks.
- Adequate ventilation in workplaces.