1. Nitrogenous Wastes Accumulation:
- Animals accumulate substances like ammonia, urea, uric acid, carbon dioxide, water, and ions (Na+, K+, Cl–, phosphate, and sulfate) through metabolic activities or excess ingestion.
2. Major Forms of Nitrogenous Wastes:
- Ammonia: Highly toxic, and requires large water amounts for elimination.
- Urea: Less toxic, excreted by mammals, terrestrial amphibians, and marine fishes.
- Uric Acid: Least toxic, excreted by reptiles, birds, land snails, and insects.
3. Ammonotelism:
- Definition:
- Excretion of ammonia, primarily in aquatic organisms.
- Excretion Process:
- Diffusion across body surfaces or gill surfaces in fish.
- Limited role of kidneys.
4. Ureotelic Animals:
- Examples:
- Mammals, some terrestrial amphibians, and marine fishes.
- Excretion Process:
- Ammonia is converted to urea in the liver.
- Urea is released into the blood, filtered, and excreted by the kidneys.
- Some urea retention for osmolarity maintenance.
5. Uricotelic Animals:
- Examples:
- Reptiles, birds, land snails, insects.
- Excretion Process:
- Excretion of nitrogenous wastes as uric acid in pellet or paste form.
- Minimal water loss.
6. Excretory Structures in Animal Kingdom:
- Protonephridia or Flame Cells:
- Found in Platyhelminthes (e.g., Planaria), rotifers, some annelids, and cephalochordates.
- Primarily for ionic and fluid volume regulation (osmoregulation).
- Nephridia:
- Present in earthworms and other annelids.
- Involved in nitrogenous waste removal and maintaining fluid and ionic balance.
- Malpighian Tubules:
- Excretory structures in insects, including cockroaches.
- Assist in nitrogenous waste removal and osmoregulation.
- Antennal Glands or Green Glands:
- Perform excretory function in crustaceans like prawns.
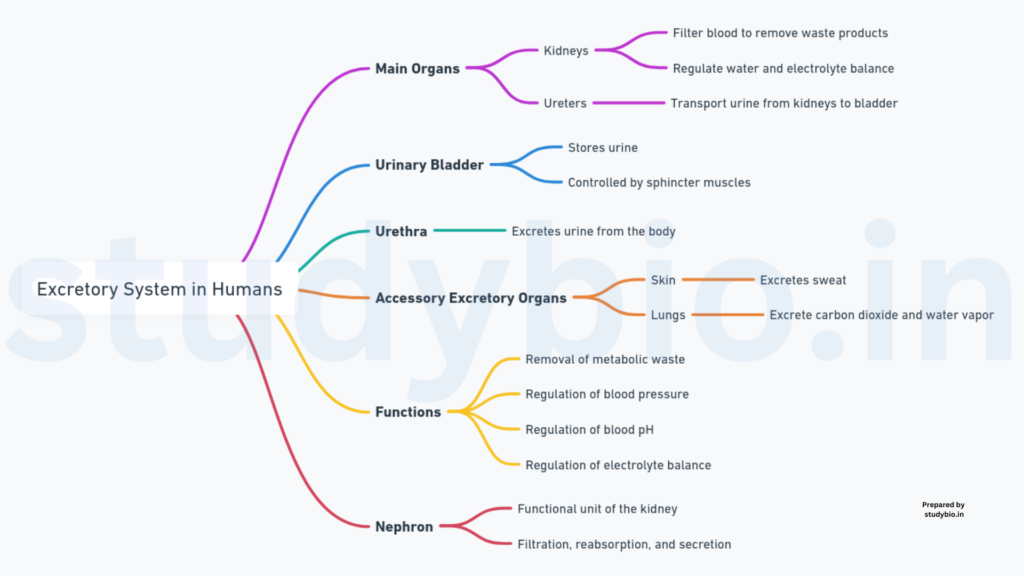
Human Excretory System
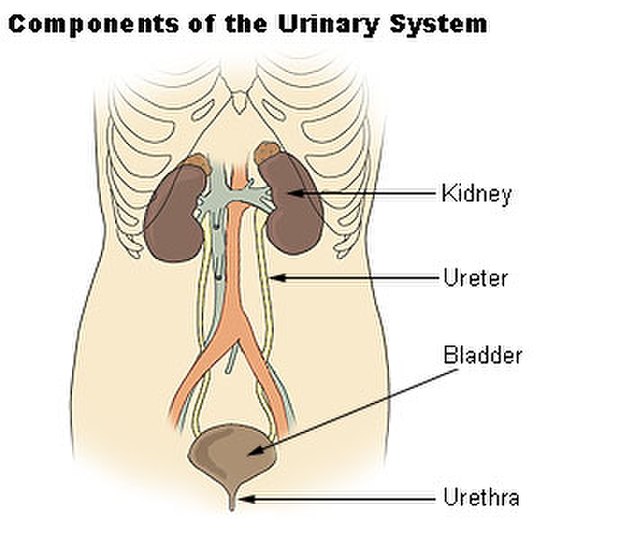
1. Components of the Human Excretory System:
- Kidneys:
- Bean-shaped organs are located between the last thoracic and third lumbar vertebrae.
- Measure 10-12 cm in length, 5-7 cm in width, and 2-3 cm in thickness.
- Average weight: 120-170 g.
- Each kidney has a hilum, a renal pelvis, and an outer capsule.
- Divided into cortex (outer) and medulla (inner).
- Ureters:
- A pair of tubes connecting kidneys to the urinary bladder.
- Urinary Bladder:
- Storage organ for urine.
- Urethra:
- The tube connecting the bladder to the external environment for urine expulsion.
2. Kidney Structure:
- Hilum:
- The notch on the inner concave surface through which the ureter, blood vessels, and nerves enter.
- Renal Pelvis and Calyces:
- Renal pelvis at the center, with calyces projecting from it.
- Capsule:
- Tough outer layer of the kidney.
- Cortex and Medulla:
- Outer and inner zones respectively.
- The medulla has conical masses (medullary pyramids) extending into calyces.
- Renal columns (Columns of Bertini) between pyramids.
- Nephrons:
- Nearly one million complex tubular structures, the functional units.
- Consists of glomerulus and renal tubule.
- Renal Corpuscle (Malpighian Body):
- Includes glomerulus and Bowman’s capsule.
- Renal Tubule:
- Begins with Bowman’s capsule and continues as the proximal convoluted tubule (PCT).
- Henle’s loop (descending and ascending limbs) and distal convoluted tubule (DCT) follow.
- DCTs of many nephrons open into a collecting duct, which converges into the renal pelvis.
- Types of Nephrons:
- Cortical Nephrons:
- The loop of Henle is short, extending minimally into the medulla.
- Juxtamedullary Nephrons:
- The loop of Henle is long, extending deep into the medulla.
- Cortical Nephrons:
3. Blood Circulation in Nephrons:
- Glomerulus:
- A tuft of capillaries formed by the afferent arteriole.
- Blood is carried away by the efferent arteriole.
- Peritubular Capillaries and Vasa Recta:
- Capillary network around the renal tubule.
- Vasa recta (U-shaped) runs parallel to Henle’s loop.
- Absent or reduced in cortical nephrons.
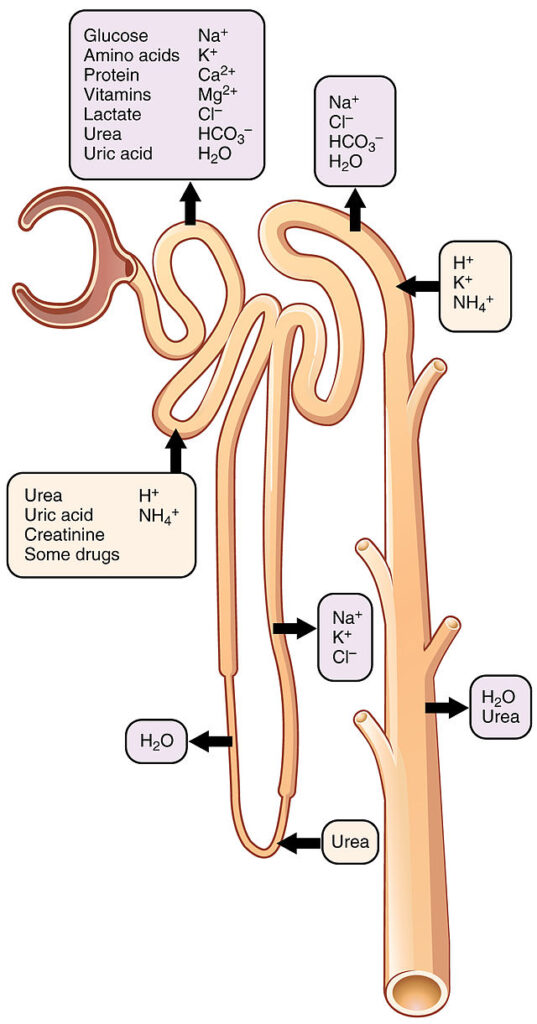
Urine Formation in the Nephron
1. Processes Involved:
- Glomerular Filtration:
- Occurs in the glomerulus.
- Filtration of blood through the endothelium of glomerular blood vessels, Bowman’s capsule epithelium, and a basement membrane.
- Podocytes in Bowman’s capsule leave filtration slits.
- Ultrafiltration process, allowing most plasma constituents except proteins to pass into Bowman’s capsule.
- Glomerular Filtration Rate (GFR): Approximately 125 ml/minute, 180 liters per day.
- Juxta Glomerular Apparatus (JGA) regulates GFR by releasing renin.
- Reabsorption:
- Nearly 99% of the filtrate (180 liters per day) is reabsorbed.
- Tubular epithelial cells in nephron segments perform active or passive reabsorption.
- Active reabsorption for glucose, amino acids, Na+, etc.
- Passive reabsorption for nitrogenous wastes and initial segments of water.
- Maintains essential substances in the body.
- Secretion:
- Tubular cells secrete H+, K+, and ammonia into the filtrate.
- Important for ionic and acid-base balance in body fluids.
- Part of the urine formation process.
2. Regulation of Glomerular Filtration Rate:
- Juxta Glomerular Apparatus (JGA):
- The sensitive region is formed by cellular modifications in the distal convoluted tubule and afferent arteriole.
- Activated by a fall in GFR, releases renin.
- Renin stimulates glomerular blood flow, restoring GFR to normal.
3. Comparison of Filtrate and Urine:
- Filtrate formed per day: 180 liters.
- Urine released: 1.5 liters.
- Signifies approximately 99% reabsorption of the filtrate by renal tubules.
Function of Renal Tubules in Urine Formation
1. Proximal Convoluted Tubule (PCT):
- Lined by simple cuboidal brush border epithelium.
- Reabsorption:
- Absorbs nearly all essential nutrients.
- Reabsorbs 70-80% of electrolytes and water.
- Maintains Balance:
- Helps maintain pH and ionic balance.
- Selectively secretes hydrogen ions and ammonia into the filtrate.
- Absorbs HCO3–.
2. Henle’s Loop:
- Role in Osmolarity:
- Minimum reabsorption in the ascending limb.
- Maintains high osmolarity of medullary interstitial fluid.
- Water and Electrolyte Transport:
- Descending limb: Permeable to water, almost impermeable to electrolytes.
- Ascending limb: Impermeable to water, allows electrolyte transport.
- Dilute the filtrate as it moves upward.
3. Distal Convoluted Tubule (DCT):
- Conditional Reabsorption:
- Reabsorbs Na+ and water conditionally.
- Selective Secretion:
- Secretes hydrogen ions, potassium ions, and NH3.
- Maintains pH and sodium-potassium balance in blood.
- Reabsorbs HCO3–.
4. Collecting Duct:
- Water Reabsorption:
- Extends from cortex to medulla.
- Reabsorbs large amounts of water, producing concentrated urine.
- Urea Passage:
- Allows passage of small amounts of urea into the medullary interstitium.
- Maintains osmolarity.
- Ionic Balance:
- Selective secretion of H+ and K+ ions.
- Maintains pH and ionic balance in the blood.
Mechanism of Filtrate Concentration in Mammals
1. Counter-Current Mechanism in Henle’s Loop and Vasa Recta:
- Opposite Flow:
- Filtrate in the two limbs of Henle’s loop flows in opposite directions.
- Blood flow in the two limbs of the vasa recta also follows a counter-current pattern.
- Proximity and Exchange:
- Proximity between Henle’s loop and vasa recta.
- The counter-current exchange maintains increasing osmolarity from the cortex to the inner medulla.
- Osmolarity Gradient:
- The gradient increases from 300 mOsmolL–1 in the cortex to about 1200 mOsmolL–1 in the inner medulla.
- Mainly caused by NaCl and urea.
2. Role of NaCl and Urea:
- NaCl Transport:
- The ascending limb of Henle’s loop transports NaCl.
- Exchanged with the descending limb of the vasa recta.
- The ascending portion of the vasa recta returns NaCl to the interstitium.
- Urea Transport:
- Small amounts of urea enter the ascending limb of Henle’s loop.
- Transported back to the interstitium by the collecting tubule.
3. Counter-Current Mechanism:
- Facilitated Transport:
- Special arrangement of Henle’s loop and vasa recta.
- The counter-current mechanism maintains a concentration gradient in the medullary interstitium.
- Interstitial Gradient:
- Facilitates easy water passage from the collecting tubule.
- Concentrates the filtrate (urine).
- Concentration Capability:
- Human kidneys can produce urine nearly four times more concentrated than the initial filtrate.
Regulation of Kidney Function
- Monitoring and Regulation:
- Monitored by hormonal feedback mechanisms.
- Involves the hypothalamus, juxtaglomerular apparatus (JGA), and to some extent, the heart.
- Osmoreceptor Activation:
- Activated by changes in blood volume, body fluid volume, and ionic concentration.
- Excessive fluid loss activates osmoreceptors.
- Stimulates the hypothalamus to release antidiuretic hormone (ADH).
- ADH facilitates water reabsorption, preventing diuresis.
- Feedback Mechanism:
- An increase in body fluid volume suppresses osmoreceptors and ADH release.
- ADH also affects kidney function through vasoconstriction, increasing blood pressure.
- Elevated blood pressure enhances glomerular blood flow and glomerular filtration rate (GFR).
- Juxtaglomerular Apparatus (JGA):
- Monitors glomerular blood flow, blood pressure, and GFR.
- Low GFR activates JG cells to release renin.
- Renin converts angiotensinogen to angiotensin I and then to angiotensin II.
- Renin-Angiotensin Mechanism:
- Angiotensin II is a vasoconstrictor, increasing glomerular blood pressure and GFR.
- Activates the adrenal cortex to release aldosterone.
- Aldosterone promotes Na+ and water reabsorption, further increasing blood pressure and GFR.
- Atrial Natriuretic Factor (ANF):
- Released with increased blood flow to the atria of the heart.
- Causes vasodilation, reducing blood pressure.
- Acts as a check on the renin-angiotensin mechanism.
Micturition: The Release of Urine
- Urine Storage:
- Urine from nephrons is stored in the urinary bladder.
- Storage continues until a voluntary signal is given by the central nervous system (CNS).
- Initiation of Micturition:
- CNS signal triggered by stretching of the bladder due to urine accumulation.
- Stretch receptors on the bladder walls send signals to the CNS.
- Motor Messages and Muscle Contraction:
- CNS transmits motor messages to initiate smooth muscle contraction in the bladder.
- Simultaneous relaxation of the urethral sphincter is induced.
- Micturition Reflex:
- The neural mechanism causes the release of urine.
- Involves coordination between CNS, bladder stretch receptors, and smooth muscles.
- Average Urine Production:
- An adult human excretes 1 to 1.5 liters of urine per day.
- Urine characteristics: light yellow, slightly acidic (pH-6.0), characteristic odor.
- Approximately 25-30 gm of urea is excreted daily.
- Clinical Significance:
- Urine analysis aids in diagnosing metabolic disorders and kidney malfunctions.
- The presence of glucose (Glycosuria) and ketone bodies (Ketonuria) in urine may indicate diabetes mellitus.
Role of Other Organs in Excretion
- Lungs:
- Remove large amounts of CO2 (approximately 200mL/minute).
- Eliminate significant quantities of water daily.
- Liver:
- Largest gland in the body.
- Secretes bile containing bilirubin, biliverdin, cholesterol, degraded steroid hormones, vitamins, and drugs.
- These substances pass out along with digestive wastes.
- Skin:
- Sweat Glands:
- Produce watery fluid containing NaCl, small amounts of urea, lactic acid, etc.
- The primary function is to facilitate body surface cooling.
- Contributes to the removal of certain wastes.
- Sebaceous Glands:
- Eliminate substances like sterols, hydrocarbons, and waxes through sebum.
- Sebum provides a protective oily covering for the skin.
- Sweat Glands:
- Overall Contribution:
- Lungs, liver, and skin collectively aid in the elimination of excretory wastes.
- Each organ plays a specific role in removing distinct types of waste products.
- This comprehensive excretory process ensures the elimination of diverse metabolic by-products from the body.
Disorders of the Excretory System
- Uremia and Hemodialysis:
- Malfunctioning kidneys lead to urea accumulation in the blood, termed uremia.
- Uremia may result in kidney failure.
- Hemodialysis Process:
- Blood is drained from an artery into an artificial kidney dialyzing unit.
- Dialysing fluid with plasma-like composition except nitrogenous wastes surrounds a cellophane tube.
- Cellophane membrane allows the movement of substances based on concentration gradients.
- Nitrogenous wastes move out into the dialyzing fluid, clearing the blood.
- After adding anti-heparin, cleared blood is pumped back into the body through a vein.
- Hemodialysis is crucial for uremic patients globally.
- Kidney Transplantation:
- The ultimate method for correcting acute renal failures.
- Functioning kidney transplanted from a donor, preferably a close relative, to minimize rejection chances.
- Modern clinical procedures enhance the success rate of this intricate technique.
- Renal Calculi:
- Formation of insoluble crystallized salt masses (oxalates, etc.) within the kidney.
- Also known as kidney stones.
- Glomerulonephritis:
- Inflammation of the kidney’s glomeruli.
- Overall Impact:
- Disorders like uremia, renal failure, kidney stones, and glomerulonephritis highlight the critical importance of kidney health.
- Medical interventions such as hemodialysis and kidney transplantation provide vital solutions to these excretory system disorders.