HUMAN REPRODUCTION
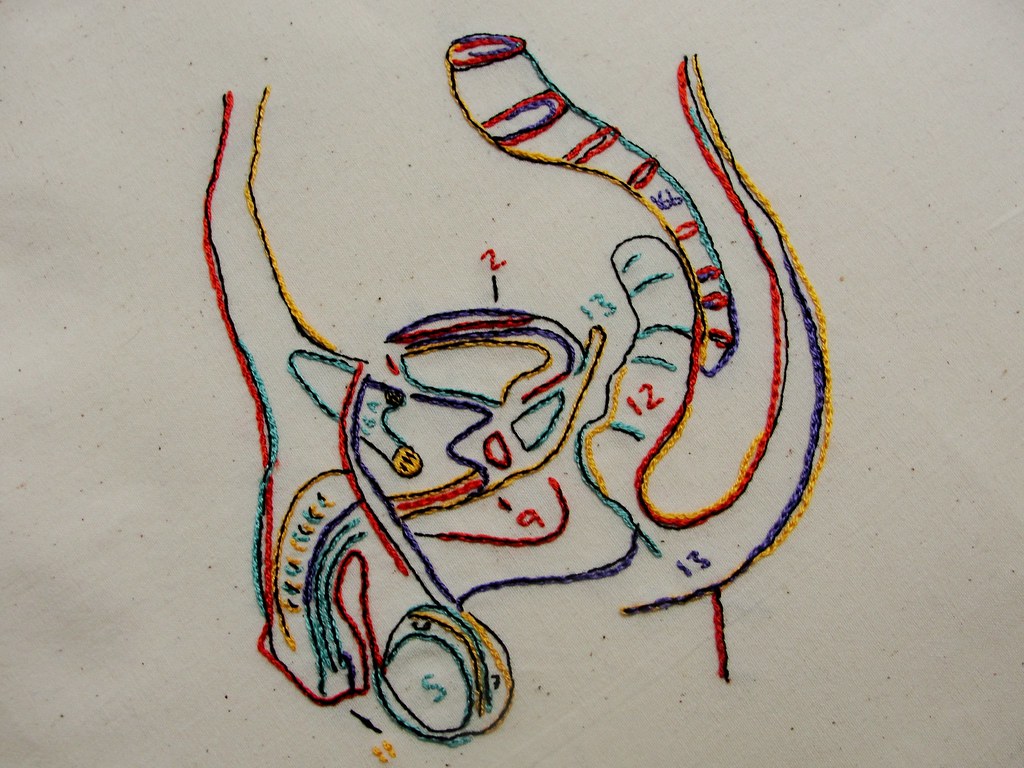
THE MALE REPRODUCTIVE SYSTEM:
The male reproductive system in humans is responsible for the production and delivery of sperm, which are necessary for fertilization of the female’s egg and the continuation of the species. It consists of several organs and structures, each with specific functions. Here is an overview of the male reproductive system:

Testes:
- The testes (singular: testis) are the primary male reproductive organs.
- They are located in the scrotum, a pouch of skin and muscle outside the abdominal cavity, which helps maintain the optimal temperature for sperm production.
- The testes produce sperm through a process called spermatogenesis.
- They also secrete testosterone, a male sex hormone responsible for the development of male secondary sexual characteristics.
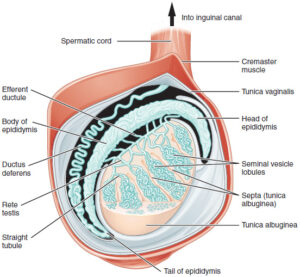
Epididymis:
- The epididymis is a coiled tube located on the posterior side of each testis.
- It serves as a storage and maturation site for sperm.
- Sperm produced in the testes travel to the epididymis, where they gain the ability to swim and fertilize an egg.
Vas Deferens (Ductus Deferens):
- The vas deferens is a muscular tube that extends from the epididymis through the inguinal canal into the pelvic cavity.
- It acts as a transport duct for mature sperm, carrying them from the epididymis to the urethra.
Urethra:
- The urethra is a duct that runs through the penis.
- It serves both the urinary and reproductive systems.
- During ejaculation, sperm travel through the urethra and exit the body through the penis.
Penis:
- The penis is the external male organ involved in sexual intercourse and the delivery of sperm into the female reproductive tract.
- It contains three cylindrical columns of erectile tissue, which fill with blood during sexual arousal, leading to an erection.
Accessory glands:
Seminal Vesicles:
- The seminal vesicles are glands located near the base of the bladder.
- They produce a significant portion of the seminal fluid (semen), which nourishes and supports sperm.
- Seminal vesicle secretions contain fructose, prostaglandins, and other substances that provide energy for sperm motility.
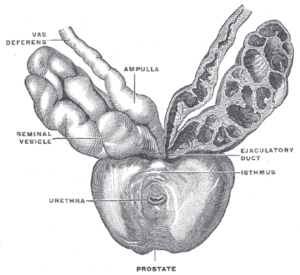
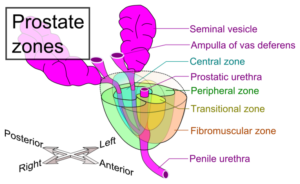
Prostate Gland:
- The prostate gland surrounds the urethra just below the bladder.
- It produces a milky, alkaline fluid that constitutes a portion of the semen.
- Prostatic fluid helps neutralize the acidic environment of the female reproductive tract, increasing sperm survival.
Bulbourethral Glands (Cowper’s Glands):
- The bulbourethral glands are small glands located at the base of the penis.
- They secrete a clear, slippery fluid that lubricates the urethra and prepares it for the passage of sperm.
- This fluid is released before ejaculation.
Puberty
Puberty is the stage of human development during which a child’s body matures into an adult’s body capable of sexual reproduction. In males, puberty typically begins between the ages of 9 and 14, although the exact timing can vary greatly among individuals. Puberty is driven by hormonal changes that lead to a wide range of physical and emotional changes in boys.
The key features of male puberty include:
Growth Spurt: One of the earliest signs of male puberty is a rapid increase in height and weight. The growth spurt typically occurs between the ages of 12 and 16, with some individual variation. Boys can grow several inches in a year during this period.
Development of Secondary Sexual Characteristics:
- Growth of Facial and Body Hair: Boys start to grow coarser, darker hair on their faces (facial hair), underarms, and in the pubic region.
- Voice Changes: The larynx (voice box) enlarges, causing the voice to deepen. This process is sometimes referred to as the “voice break.”
- Muscle Growth: Increased levels of testosterone, a male sex hormone, lead to muscle development and a more masculine physique.
- Development of Adam’s Apple: The enlargement of the Adam’s apple is another effect of the growth of the larynx.
Genital Development:
- Enlargement of the Testes: The testes grow in size and become more active, producing sperm and the male sex hormone testosterone.
- Penis Growth: The penis also increases in size.
Acne and Skin Changes: Increased oil production in the skin can lead to acne. Boys may also experience changes in skin texture.
Emotional and Behavioral Changes: Hormonal changes can lead to emotional ups and downs. Adolescents may experience mood swings, increased aggression, and heightened interest in sexual matters.
Reproductive System Activation: The testes begin to produce mature sperm during puberty. Boys start experiencing erections and spontaneous ejaculations, often during sleep (nocturnal emissions).
Gynecomastia: Some boys may experience temporary breast enlargement (gynecomastia) due to hormonal fluctuations. This typically resolves on its own.
Sexual Awareness: As sexual maturity progresses, boys become more aware of sexual feelings and may begin to have sexual attractions.
Cognitive and Psychological Changes: Adolescents often experience cognitive development and changes in their thinking processes. They may also develop a sense of identity and autonomy.
The duration and progression of puberty can vary widely between individuals. While some boys may complete the process in a few years, for others, it can take several years. The entire puberty process generally lasts from around ages 9 to 16, with variations.
Spermatogenesis
Spermatogenesis is the process by which sperm cells (spermatozoa) are produced in the testes of male animals, including humans. It is a complex and highly regulated biological process that involves the proliferation and differentiation of germ cells (spermatogonia) into mature sperm cells. Here’s an overview of spermatogenesis in humans:
Location: Spermatogenesis primarily occurs in the seminiferous tubules of the testes, which are coiled structures within the testicular tissue.
Stages of Spermatogenesis: Spermatogenesis can be divided into several stages, including:
a. Spermatogonial Phase: The process begins with spermatogonia, which are diploid stem cells. These cells undergo mitotic divisions to give rise to more spermatogonia, ensuring a continuous source of germ cells.
b. Meiotic Phase: Spermatogonia undergo meiosis to produce haploid cells. The first meiotic division (meiosis I) reduces the chromosome number from diploid (2n) to haploid (n), and the second meiotic division (meiosis II) further refines the genetic material.
c. Spermiogenesis: The haploid cells resulting from meiosis are called spermatids. During spermiogenesis, these spermatids undergo extensive morphological changes, including the development of a tail (flagellum) and the condensation of genetic material into a compact form. The end product of spermiogenesis is a mature sperm cell (spermatozoon).
Sperm Maturation: While spermatogenesis begins during puberty, sperm maturation is not complete at that time. Sperm must travel through the epididymis, where they acquire motility and the ability to fertilize an egg. The process of sperm maturation can take several weeks.
Sperm Transport: Once matured, sperm are stored in the epididymis and are transported to the vas deferens during ejaculation. From there, they can be expelled from the male’s body during sexual intercourse.
Spermatogenesis Regulation: The process of spermatogenesis is regulated by hormones, primarily follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are produced by the pituitary gland in response to signals from the hypothalamus. FSH stimulates the development of sperm cells, while LH stimulates the Leydig cells in the testes to produce testosterone.
Sperm Production Rate: The rate of sperm production can vary among individuals but is typically in the range of hundreds of millions of sperm per day.
Sperm
Sperm is the male gamete or sex cell in humans and many other animals. It is a specialized cell designed for the purpose of fertilizing an egg (ovum) during sexual reproduction. Sperm cells are produced through the process of spermatogenesis, as previously described, and have a unique structure adapted for their specific function. Here is an overview of the structure of a sperm cell:
Sperm Structure:
Head: The head is the front part of the sperm cell and contains the nucleus. It is covered by a cap-like structure called the acrosome, which contains enzymes that help the sperm penetrate the egg’s protective layer during fertilization.
Nucleus: The nucleus contains the genetic material (chromosomes) necessary for fertilization. It combines with the nucleus of the egg to form the zygote, which is the initial cell of the new organism.
Midpiece: The midpiece is the region behind the head and is packed with mitochondria. Mitochondria are the powerhouses of the cell and provide energy (in the form of ATP) for the sperm’s movement.
Tail (Flagellum): The tail is a long, whip-like structure extending from the midpiece. It is responsible for the sperm’s motility or swimming ability. The tail propels the sperm forward, allowing it to swim through the female reproductive tract in search of the egg.
Elongated Shape: Sperm cells have an elongated, streamlined shape that aids in their movement through the female reproductive tract.
Sperm Function:
Sperm’s primary function is to fertilize an egg during sexual reproduction. The process of fertilization involves several steps:
Ejaculation: Sperm are released from the male’s testes and epididymis into the female’s reproductive tract during ejaculation.
Swimming to the Egg: Sperm swim through the cervix, uterus, and fallopian tubes in the female reproductive tract. This journey can take several hours to several days.
Fertilization: If sperm reach an egg in the fallopian tube, the acrosome releases enzymes to help the sperm penetrate the egg’s outer layer. Once the sperm successfully enters the egg, their nuclei fuse, resulting in a fertilized egg (zygote).
Zygote Formation: The zygote begins to divide and develop into an embryo, which eventually implants in the uterus for further development.
Sperm are highly specialized for their role in fertilization, as they need to traverse a challenging and complex journey to reach the egg and successfully fertilize it. It’s essential to have viable and motile sperm for natural conception. Various factors, including sperm count, motility, and morphology, can affect a man’s fertility and the likelihood of fertilization.
Hormonal regulation of Spermatogenesis in Human Male
Spermatogenesis in human males is a complex and highly regulated process that is hormonally controlled. The primary hormones involved in the hormonal regulation of spermatogenesis are as follows:
Gonadotropin-Releasing Hormone (GnRH):
- GnRH is released by the hypothalamus in the brain.
- It stimulates the anterior pituitary gland to produce and release two important hormones: luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
Luteinizing Hormone (LH):
- LH is produced and released by the anterior pituitary gland.
- LH stimulates the Leydig cells in the testes to produce and release testosterone, a key hormone for spermatogenesis.
Follicle-Stimulating Hormone (FSH):
- FSH is also produced and released by the anterior pituitary gland.
- FSH acts directly on the Sertoli cells in the seminiferous tubules of the testes.
Testosterone:
- Testosterone is the primary male sex hormone produced by the Leydig cells in the testes.
- It is essential for the initiation and maintenance of spermatogenesis.
- Testosterone influences the development of secondary sexual characteristics, such as facial and body hair, deepening of the voice, and muscle development.
Hormonal Regulation of Spermatogenesis:
The release of GnRH from the hypothalamus initiates the process. GnRH stimulates the anterior pituitary gland to secrete LH and FSH.
LH acts on the Leydig cells in the testes, promoting the production and release of testosterone. Testosterone is crucial for initiating and maintaining spermatogenesis.
FSH acts on the Sertoli cells within the seminiferous tubules of the testes. Sertoli cells provide physical and nutritional support to developing sperm cells (spermatogonia) and help regulate the process of spermatogenesis.
Under the influence of FSH and testosterone, spermatogonia undergo mitotic divisions and develop into mature sperm cells (spermatozoa) through the processes of meiosis and spermiogenesis.
Testosterone also has a role in regulating the size and function of the male accessory reproductive organs, including the seminal vesicles, prostate gland, and bulbourethral glands.
The entire process of spermatogenesis, from the initiation of sperm production to the release of mature sperm into the epididymis, is regulated by this intricate hormonal system. Spermatogenesis is a continuous process in males that typically starts at puberty and continues throughout their reproductive years.
The coordinated actions of GnRH, LH, FSH, and testosterone ensure that sperm production is maintained, allowing for the continual production of male gametes needed for sexual reproduction.